The district hospital doctors were worried about this child, a 10-month old girl with a serious respiratory infection. They were treating her for pneumonia as well as for TB, but every day her breathing continued to worsen. She was tiny for her age, but despite receiving extra nutrition she did not gain any weight. Eventually the doctors decided to send her along with her mother to the capital.
After about 8 hours on the road the mother and child reached the government hospital in Dili. Sometimes patients from remote districts have family in Dili who can provide support, but in this case the young mother knew no one. It is not difficult to imagine her anxiety, sitting by the bedside as her child struggled to breathe. The government hospital doctors tried giving various antibiotics, but there were no signs of improvement.
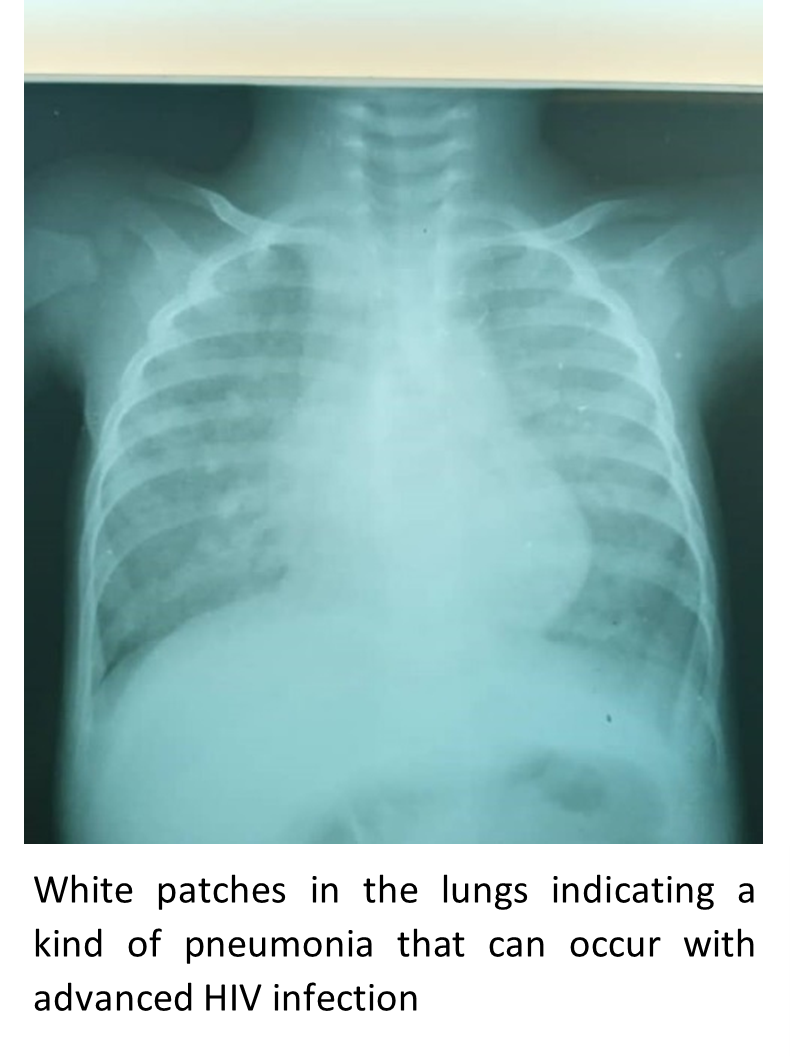
Then a trainee doctor rotated onto the Paediatric ward. After reviewing the case (including the chest X-ray shown), she recommended the test that would save the child’s life – an HIV test. The child’s test was positive, and when tested later both parents were also found to have HIV.
With this information, the trainee doctor realised that the child had a particular sort of pneumonia that occurs when HIV weakens the immune system. Once changed over to the correct antibiotic the child’s condition quickly improved.
It is not so easy to imagine the mother’s frame of mind at this point. Relief, that the cause of the problem had been found and that her child could breathe normally again. Perhaps guilt? We hear this commonly from HIV positive mothers, although they have passed the virus to their children unknowingly, as their husbands have unknowingly passed it to them. And fear – of an early death, and of becoming a social outcast if her HIV positive status were to become known in her community.
Because of this trainee doctor’s insight in requesting the HIV test, the child has now recovered from her pneumonia and she is gaining weight. She and her parents can start the anti-HIV therapy which should see them living long and healthy lives.
We in the Maluk Timor HIV program are proud of this positive outcome – because we were the ones who supervised the trainee doctor. Last year she did a 2-week placement in our HIV Centre and took some simple but powerful knowledge away with her – how to interpret a chest x-ray, which test to do, which drug to give. This knowledge allowed her to save the lives of three people that would otherwise have been lost.
This young doctor is one of 36 who have done short HIV clinical placements with us so far. These 36 doctors have been trained by the six outstanding Timorese health workers forming the Maloa HIV Care Team, who in turn have been trained by Maluk Timor volunteers.
Our model is based on the belief that the knowledge and confidence we impart will expand outwards, as those we train will in turn share their knowledge with others. Only by empowering the Timorese health workers in this way can our efforts have a sustainable impact into the future.
Our HIV Program is based in Dili, and it comprises a mix of both Maluk Timor and Ministry of Health staff forming one unit. From having no HIV experience two years ago, these six team members now provide care for many HIV positive patients independently, while seeking back-up from Maluk Timor volunteer clinicians to help with complex cases.
For the Maloa HIV Team, providing patient care and providing education are not separate activities but concurrent. The team’s knowledge is growing rapidly as they continue to enrol HIV patients and deal with new situations, and they are then sharing their experience with other Timorese workers.
During the two years since we started our program, we have enrolled 160 patients living with HIV. It is a testament to the friendliness and dedication of our team members that 97% of patients have remained in care with us. Stigma and discrimination against people living with HIV is rampant in Timor-Leste, including within the healthcare system, such that drop-out from care is common in other settings.
At 3% our mortality rate is substantially lower than that expected for people with HIV in other parts of the country, and it reflects the quality of the care that we provide. This mortality rate is remarkable when you consider that over 40% of our patients have advanced HIV disease at the time of their enrolment.
To address this problem of late HIV diagnosis we emphasise the importance of early testing during our HIV training workshops around the country. Late HIV diagnosis means both higher mortality as well as expansion of the epidemic since undiagnosed people with HIV are not yet on treatment and so are infectious to others.
Maluk Timor has provided HIV training workshops for over two hundred health workers in Dili and in also remote districts. This step towards decentralisation of HIV care is a crucial one since health services are currently concentrated in the capital, while around three quarters of the population of Timor-Leste live in remote mountainous districts.
Ongoing care for this newly diagnosed HIV positive family will be a challenge since there are no doctors near their village with knowledge of how to prescribe HIV medicine. They will need to keep visiting Dili for their medical care which will only be possible if they can find the $12 each way for bus fare. For many such HIV positive families in Timor-Leste $12 is far (and fatally) out of reach.
Prevention of mother-to-child transmission of HIV is a key priority for the Ministry of Health, and it is an area where Maluk Timor is well placed to provide support. If the 10-month old’s mother had been tested and treated for HIV during pregnancy, then her child would likely not have become infected. Unfortunately, many health workers in remote districts have not yet been trained in this routine step.
Ultimately, we hope that the model of care we are demonstrating at Maloa can be expanded, with a view to improving the standard of HIV care across the country.
There is an urgency to this plan since the rate of new HIV infections is quickly increasing here. This rapid rise in incidence presents an impending public health crisis which will be disastrous for the country if the trend cannot be turned around before the epidemic becomes generalised.
With your support we hope to seize this crucial window of time and act with energy and passion to assist the Ministry of Health with implementation of effective HIV programs for Timor-Leste.
What have we achieved to date? Since the HIV Care Centre opened in November 2018, we have:
- Enrolled 160 patients, with 94% of those started on anti-HIV treatment supported to stay on treatment
- Widely promoted HIV prevention strategies including HIV testing and use of condoms
- Provided intensive HIV training/mentoring to a core team of 6 Timorese health workers (the Maloa HIV Team)
- Provided basic HIV training to over 200 Timorese health workers around the country including remote centres
- Collaborated with the Ministry of Health and other key partners to develop national HIV strategies and training programs
What would we like to do next?
- Build a new, larger, fit-for-purpose HIV Care and Training centre
- Continue to diagnose and manage patients with HIV infection
- Continue to provide HIV training to more Timorese community health care workers, including midwives as part of the Prevention of Mother-To-Child Transmission of HIV campaign
- Continue to upskill our core HIV Team, including providing the opportunity for two of them to attend an international HIV academic conference
- Expand community engagement activities e.g. sharing of accurate HIV messaging on TV/radio/social media
- Purchase a vehicle for HIV program to enable home visits and looking for lost-to-follow-up patients
- Provide social support for patients e.g. travel costs
How can donors support? Financial or in-kind support for any of the above.
| USD | AUD | |
| Establish a new, larger HIV care and training centre | $130,000 | $200,000 |
| Annual running costs of existing program | $39,000 | $60,000 |
| Employ additional Timorese clinical staff | $26,000 | $40,000 |
| Purchase a vehicle for HIV program | $13,000 | $20,000 |
| Social support to patients (one year) | $3,250 | $5,000 |